We have listed our most commonly asked questions here. If you would like to see a particular question answered in this section, please contact us and we will add it to the list.
|
This website uses cookies to allow us to understand our visitors and provide the best experience and information. If you prefer, you can turn off cookies in your browser.
Access to this website is also based on acceptance of our Terms of Use. |

We have listed our most commonly asked questions here. If you would like to see a particular question answered in this section, please contact us and we will add it to the list.
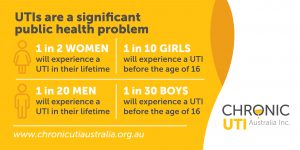
Women are the most common group afflicted by UTIs. However, UTIs also affect babies, children, men and especially the elderly.
UTIs are common in otherwise healthy adult women, but there are some medical conditions that can increase their likelihood. These include diabetes, conditions causing immunosuppression, physical injuries impacting the spine/pelvis and conditions requiring catheterisation1.

1 Foxman, B., Epidemiology of urinary tract infections: Incidence, morbidity, and economic costs. Disease-a-Month, 49(2), 53-70, 2003; doi: 10.1016/S0011-5029(03)90000-9 www.ncbi.nlm.nih. gov/pubmed/12601337
An estimated 50% of all women will experience an acute UTI in their lifetime2. This means, even if you have not had a UTI yourself, someone close to you has. To explain the difference between an acute and chronic UTI, we need to delve into some science.
During an acute UTI, pathogenic bacteria invade the urethra/bladder and multiply rapidly in the urine. This is known as a planktonic infection. An acute (planktonic) UTI will result in the sudden onset of one or more of the distressing UTI symptoms most Australian women are familiar with—painful urination (dysuria), urgency, extreme frequency, excruciating bladder/lower abdominal pain, lower back pain and, sometimes, cloudy, smelly or even blood-filled urine.
A chronic UTI presents differently because the bacteria have become embedded within the lining of the bladder/urinary tract. Anyone who has an acute UTI is at risk of the infection becoming chronic. In fact, most people with a chronic UTI can clearly pinpoint the origins of their symptoms after an acute UTI did not fully resolve after treatment. This is because, in some circumstances when treating an acute UTI, bacteria can evade the host immunity or antibiotic attack. For safety, they cleverly burrow into the cells that form the bladder lining (known as the urothelium) and/or gather in tight clusters covered in a sticky substance called biofilm. Once embedded in the urothelium, the infection becomes increasingly difficult to diagnose using current testing tools and is challenging to treat3,4.

2 Foxman, B. (2003). Epidemiology of urinary tract infections: Incidence, morbidity, and economic costs. Disease-a-Month, 49(2), 53-70. doi: 10.1016/S0011-5029(03)90000-9 www.ncbi. nlm.nih.gov/pubmed/12601337
3 Professor James Malone-Lee, Emeritus Professor of Nephrology, University College London, personal communication, 27 January 2018 www.chronicutiaustralia.org.au/chronic-uti/how-chronic-uti-forms/ Accessed 15 September 2018
4 Rosen DA, Hooton TM, Stamm WE, Humphrey PA, Hultgren SJ., Detection of intracellular bacterial communities in human urinary tract infection. PLoSMed. 2007;4(12):e329 www.ncbi.nlm.nih.gov/pubmed/15337164
Chronic UTI can present in several ways. It can occur as recurrent acute UTIs, often increasing in frequency and severity over time. Alternatively, chronic UTI can feature constant background urinary symptoms (that usually appear negative on dipsticks and MSU culture tests) and acute attacks known as ‘flares’.
Chronic UTI symptoms can include some, or all, of the symptoms experienced during an acute UTI, along with chronic bladder/pelvic pain, urethral/vulval pain, overactive bladder, stress urinary incontinence, voiding problems and frequency symptoms. Typically, people with chronic UTI will suffer these painful, relentless and often debilitating symptoms for many years or even entire lifetimes.
There are two tests currently used to diagnose UTIs that were developed and introduced in the 1950s—the urinary dipstick and the MSU culture. There is also a new form of UTI testing, molecular (DNA) testing, which has recently become commercially available through several labs in the United States.
The urinary dipstick is used by doctors as a basic first-line diagnostic tool. It is designed to pick up signs of an acute UTI, such as leukocyte esterase (signs of pus/white blood cells), nitrites (produced by some types of gram negative bacteria) and blood. Urinary dipsticks have been widely discredited, with research showing they miss up to 70% of infections6,7,8. They can be useful in confirming a clearly positive acute infection,
but dipsticks are ineffective at ruling out infection.

Cultures are performed in clinical labs to grow and identify the bacteria responsible for an infection. They are also used to determine any antibiotic resistance the identified bacteria may harbour. The MSU culture was originally developed to diagnose pyelonephritis (a kidney infection)—a much more severe and serious form of acute upper urinary tract infection.
Although the culture, along with its set of arbitrary diagnostic thresholds, was never validated for diagnosing acute UTIs, it somehow became adopted worldwide as the ‘gold standard’ tool for UTI diagnosis. For the past 30 years, researchers have been demonstrating that MSU culture tests are fundamentally flawed and miss 50–80% of UTIs8,9.
Traditionally, culture testing has been mostly satisfactory for the majority of uncomplicated, acute UTIs caused by Escherichia coli (E. coli), and several other known urinary pathogens. However, research shows this ‘gold standard’ test fails to diagnose chronic UTI, complicated and polymicrobial UTIs, lower grade UTIs and infections caused by more recently recognised uropathogens10.

DNA-based molecular testing for diagnosing UTIs is generating interest because of its ability to identify all bacteria in a urine sample. There are now several labs in the United States offering DNA UTI testing for international customers (testing technologies and costs vary between labs).
There is no consensus on the value of DNA-based molecular testing in diagnosing chronic UTIs. Some research experts are critical due to the current lack of understanding of the urinary microbiome and the inability to describe the microbes truly responsible for health and disease. In Australia, anecdotal reports so far highlight difficulties for people finding practitioners who understand the test results and have specialist knowledge in treating chronic UTI.
Although it is still early days, it is hoped that molecular testing will one day allow the identification of a personalised healthy urinary microbiome and inform future treatment options.
-Learn More About UTI Testing Here
5 Diagnosing UTIs is ‘a dog’s breakfast,’ and that’s affecting women, The Current, CBC.CA, 3 April 2018, Radio www.cbc.ca/player/play/1201579075817. Accessed 15 September 2018.
6 Khasriya R, Khan S, Lunawat R, Bishara S, Bignal J, Malone-Lee M, et al. The Inadequacy of Urinary Dipstick and Microscopy as Surrogate Markers of Urinary Tract Infection in Urological Outpatients With Lower Urinary Tract Symptoms Without Acute Frequency and Dysuria. JUrol. 2010;183(5):1843-7. www.ncbi.nlm.nih.gov/pubmed/20303096
7 Kupelian AS, Horsley H, Khasriya R, Amussah RT, Badiani R, Courtney AM, et al. Discrediting microscopic pyuria and leucocyte esterase as diagnostic surrogates for infection in patients with lower urinary tract symptoms: results from a clinical and laboratory evaluation. BJU Int. 2013;112(2):231-8. doi: 10.1111/j.1464-410X.2012.11694.x. PubMed PMID: 23305196. www.ncbi.nlm.nih.gov/pubmed/23305196
8 Brubaker L, Wolfe AJ. The Female Urinary Microbiota/Microbiome: Clinical and Research Implications. Rambam Maimonides medical journal. 2017;8(2). Epub 2017/05/04. doi: 10.5041/rmmj.10292. PubMed PMID: 28467757; PubMed Central PMCID: PMCPMC5415361. www.ncbi.nlm.nih.gov/pubmed/28467757
9 Gill K, Kang R, Sathiananthamoorthy S, Khasriya R, Malone-Lee, J. A blinded observational cohort study of the microbiological ecology associated with pyuria and overactive bladder symptoms. Int Urogynecol J. 2018. Epub 2018/02/20. doi: 1007/s00192-018-3558-x. PubMed PMID: 29455238. www.ncbi.nlm.nih.gov/pubmed/29455238
10 Price, TK, Hilt EE, Dune TJ, Mueller ER, Wolfe AJ, Brubaker L., Urine trouble: should we think differently about UTI? International Urogynecology Journal doi.org/10.1007/s00192-017-3528-8, www.ncbi.nlm.nih.gov/pubmed/29279968
Compared with acute UTI, chronic UTI involves lower numbers of bacteria that invade the bladder lining and move in and out of a dormant (quiescent) state. These lower level bacterial loads will most likely fall well below the thresholds set for diagnosing acute UTI and are interpreted as ‘negative’11. Since chronic UTI is not a recognised condition, there has been no drive to introduce a second level test to diagnose UTIs that fall outside the existing diagnostic criteria (which were originally designed for diagnosing pyelonephritis).
11 Professor James Malone-Lee, Emeritus Professor of Nephrology, University College London, personal communication, 27 January 2018 www.chronicutiaustralia.org.au/chronic-uti/how-chronic-uti-forms/ Accessed 15 September 2018
At the Artemis Cystitis Clinic (10 Harley Street, London), a chronic UTI diagnosis is based on a patient’s symptoms, history and signs of infection found by microscopy looking at an immediately fresh, unspun, unstained and undiluted urine sample. The microscopy is looking for evidence of white blood cells (pus cells fighting infection) and epithelial cells (shedding of the bladder lining as part of the natural immune response). Professor Malone-Lee is the author of ‘Cystitis Unmasked’. You can learn more in our 2021 interview with Professor Malone-Lee here.

The late Professor Malone-Lee’s Artemis Cystitis Clinic is located at 10 Harley Street, London W1G 9PF. The clinic accepts international patients and offers assessment, diagnosis and treatment supported by fresh urine microscopy. The management programme is based on the research findings coming out of his academic programme at UCL. You can find out more about the clinic’s diagnostic and treatment protocol by contacting the administration team at the Artemis Cystitis Clinic, email: ClinicAdministration@ArtemisCystitis.com or by telephone from Monday to Friday 9.30am – 5.30pm: 07568 403211, or visit there website launched in October 2024 here: https://artemiscystitis.co.uk/
Dr Rajvinder Khasriya, who heads the NHS LUTS Service at Whittington Hospital and previously worked at Professor Malone-Lee’s private clinic, now offers consultations to international patients at her private clinic, Chronic UTI @ The Portland, London. You can learn more about the clinic here or by emailing the practice manager Ali Parkes, email: uti.portland@hcahealthcare.co.uk .
You can also read-up on the LUTS treatment protocol in the following research papers, published 2018:
Recalcitrant chronic bladder pain and recurrent cystitis but negative urinalysis: What should we do?
Along with the FAQ page for the NHS Clinic at the Whittington Hospital, London, which offers the same chronic UTI treatment as the private Artemis Cystitis Clinic at 10 Harley Street, London.
You can read a published opinion piece by Professor Malone-Lee published in the British Medical Journal in 2018:
Urinary infections are complex and hard to treat.
This is absolutely true. Urine is not sterile12. This discovery is proving to be one of the biggest myth busters of the 21st century when it comes to bladder health and disease. As recently as 2012, scientists in the United States discovered a residential microbial community within the bladders of healthy women—dubbed the female urinary microbiota (FUM). Using DNA testing, researchers were able to identify over 400 different bacterial species living in both healthy women and women with lower urinary tract symptoms. Some of these species are thought to be beneficial and perform a protective role within the bladder.
This discovery is important because the traditional understanding of urinary infections, and the foundation that UTI tests are built on (in the 1950s), assumes healthy urine is sterile—and an isolated ‘known’ urinary pathogen (grown by culture) is responsible for infection. This is no longer the case. The discovery of the urinary microbiota is forcing scientists, microbiologists and clinicians to re-think everything previously accepted about bladder health and disease, including what causes UTIs and other urinary disorders—such as interstitial cystitis/painful bladder syndrome (IC/PBS), over active bladder syndrome (OAB) and urgency urinary incontinence (UUI)—and how these conditions are best diagnosed and treated.

12 Wolfe AJ, Toh E, Shibata N, et al. Evidence of uncultivated bacteria in the adult female bladder. J Clin Microbiol. 2012;50(4):1376-1383, jcm.asm.org/content/50/4/1376.full
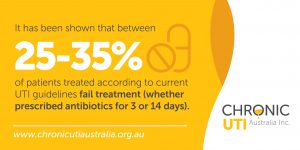
Scientists have not yet reached a consensus as to why 25–35% of people with an acute UTI fail the standard antibiotic therapy prescribed13. However, researchers have shown that bacteria, such as E. coli, are able to communicate between themselves via a process known as ‘quorum sensing’. Such communication enables them to form biofilm-like intracellular bacterial communities early on during an acute infection, leaving behind a bacterial reservoir capable of seeding future acute attacks and/or ongoing lower urinary tract symptoms14.
13 Zalmanovici TA, Green H, Paul M, Yaphe J, Leibovici L. Antimicrobial agents for treating uncomplicated urinary tract infection in women. CochraneDatabaseSystRev.2010;(10):CD007182, cited in Malone-Lee J, Urinary infections are complex and hard to treat, BMJ 2017;359:j4784 www.bmj.com/content/359/bmj.j5766.full?ijkey=IiTCSBtWau0sm9j&keytype=ref
14 Opal SM, Communal Living by Bacteria and the Pathogenesis of Urinary Tract Infections. PLoS Med. 2007 Dec; 4(12): e349. Published online 2007 Dec 18; doi: 10.1371/journal. pmed.0040349 www.ncbi.nlm.nih.gov/pmc/articles/PMC2140084/
Presently, long-term, full-dose antibiotic therapy is the only readily effective treatment for people diagnosed with chronic UTI15. You can read more about this, including a supporting study on our Treatment page. Researchers are desperately searching for fast, effective and safe alternatives to traditional antibiotics.
• Bacteriophage therapy (using viruses to attack pathogenic bacteria).
• Probiotics to return the urinary microbiota to a healthy state.
• Vaccination against select urinary pathogens.
• Super-strength mannosides to stop bacteria from becoming embedded in the bladder wall.
• New nanoparticle technology that administers the antibiotic directly into the bladder where it can reach uropathogens protected by biofilm and/or hiding inside the cells that line the bladder.
15 Swamy, S., Barcella, W., Iorio, M., Gill, K., Khasriya, R., Kupelian, A., ., Rohn, JL., Malone-Lee, J., Recalcitrant chronic bladder pain and recurrent cystitis but negative urinalysis: What should we do? International Urogynecology Journal, 29(7), 1035-1043; 2018; doi: 10.1007/s00192-018-3569-7 link.springer.com/article/10.1007/s00192-018-3569-7
Because chronic UTI is a poorly recognised condition that has no accurate diagnostic test, most people fail to achieve a proper diagnosis.

Commonly, people with chronic UTI are diagnosed with incurable ‘urinary syndromes’ like interstitial cystitis/painful bladder syndrome (IC/PBS), overactive bladder syndrome (OAB) or urinary urge incontinence (UUI). Diagnosis of a ‘urinary syndrome’ is usually made after seeking help from three to five different practitioners over a period of three to seven years16.

Chronic UTI is a debilitating condition. Many people with an untreated chronic UTI live with symptoms of distressing and incapacitating pain and constant urinary frequency and urgency—all of which significantly impact psychological and emotional health and wellbeing. If left untreated, chronic UTI ruins lives, relationships, self-confidence and the ability to work, be sexually intimate and manage families.

16 Interstitial Cystitis Fact Sheet, Women’s Health Queensland Wide, www.womhealth.org.au Accessed 27 February 2018
– Read Dozens of First Hand Stories by Recovered Chronic UTI Patients
– Subscribe to Our Blog and a New Patient Story will be Delivered to your Inbox Monthly
In Australia, there are currently no tests or treatment guidelines for chronic UTI. Not all doctors recognise chronic UTI as a disease or know how to treat it, so practitioners often vary in their approach.
However, there are Australians being treated for chronic UTI who have proactively researched the disease and partner with their doctor to treat their embedded infection using antimicrobials, traditional Chinese medicine or natural therapies.
How can you find out more?
You can talk to some of these people, and others who are researching and undergoing various therapies, in a number of online support/chat groups for chronic UTI. Please search on Facebook or contact us for a current list from the growing global network.
You can read more from others who have cured their chronic UTI using a variety of approaches on the Chronic UTI Australia recovery blog. By subscribing to our blog, you will receive a free copy of our Understanding Chronic UTI booklet in PDF, plus a positive, real-life patient story will be delivered direct to your inbox. Click here to subscribe.
www.icinfocenter.wordpress.com
– Read Tips From Australians Who Have Successfully Sought Treatment For Chronic UTI
We are asked this question more than any other!
Chronic UTI Australia Incorporated does not endorse any particular treatment protocol for chronic UTI and we are prevented from making doctor recommendations. There are currently no practitioners in Australia that specialise in diagnosing and treating chronic UTI that we know of. However, there are a growing number of Australians being diagnosed and successfully treated for chronic UTI by either an international specialist or their own GP, urologist or treating microbiologist. It is important to note that feedback from chronic UTI patients who have success accessing treatment say they partner with their existing GP. We completely understand that this depends on the relationship you have with your current GP. Please visit our page ‘What to do if you think you have a chronic UTI’ for suggestions on how to prepare for a conversation with your GP.
We suggest connecting with others who are being treated for chronic UTI. You can read some of their stories on our blog or talk to them in one of the many chat groups we list in the FAQ below. There are various other UTI groups you can find through a Facebook search, by asking in one of the groups listed, or by reading more on this post Who Treats Chronic UTI?.
Chronic UTI Australia Incorporated does not own or manage any online support/information chat groups. However, we are familiar with a number of popular groups but we cannot vouch for the quality and accuracy of the information or their administration.
Please be aware that mostly members in these group are not medically trained or qualified and they do not offer medical advice. Online support and information groups are not intended to replace a one-on-one relationship with a qualified healthcare professional. Members within the groups share and discuss their own experiences and research in good faith. You are encouraged to make your own healthcare decisions based upon your own research and in partnership with a qualified healthcare professional.
To make sure any of the following online support/information groups are right for you, please first do some research.
Chronic and Recurrent UTI Chat Group (Australia and New Zealand
(This is a ‘private’ group that accepts residents of Australia and New Zealand only. This group focuses on science-based discussions about treatment for chronic UTI and is for women and men.)
Embedded UTI Advice and Support Group
(This is a large ‘private’ group that is UK-based with many international members. This group focuses on science-based discussions about treatment for chronic UTI and is for women and men.)
Everyday Wellness Support Group – Stop UTI Forever
(A large group that focuses mostly on natural UTI therapies and anecdotal evidence.)
Chronic UTI Women’s Support Group
Men and Women’s Chronic UTI Support Group
Support Group for UTIs in Children
(The above three ‘private’ groups are run by the UK-based patient advocacy organisation ‘Chronic Urinary Tract Infection Campaign’ or CUTIC UK. The first group was established in 2013 and there are many members with good knowledge and experience who are being treated by various chronic UTI doctors in the United Kingdom. Discussions vary around treatment approaches and not all treatment protocols are science-based.)
(This is a large ‘private’ UK-based group for people who have been diagnosed with vaginal atrophy [VA], with many current members who have chronic UTI and VA.)
(This site offers forums for various bladder health related topics. The forums are public so please make sure you select an anonymous identity when signing up to join.)
(This site offers forums for various topics, including various UTI forums.)
Table of Contents
×A young adult writes of her experiences as a child:
“I developed a chronic UTI as a result of recurrent childhood urinary infections which were repeatedly misdiagnosed and left untreated, resulting in severe bladder and kidney symptoms which left me with a diagnosis of interstitial cystitis. I am now 22 years old and this condition has stripped me of my entire childhood.
“I started to develop symptoms of severe urinary frequency and urgency when I was 6 years old. When my parents initially took me to see my GP, a urine dipstick was carried out and showed no signs of infection. A subsequent culture showed insignificant bacterial growth, resulting in no further treatment. When my symptoms subsequently worsened over the next 3 months, further negative dipsticks and cultures were carried out and I was misdiagnosed with overactive bladder syndrome. By this time, my urinary frequency had progressed to the point where I was urinating every 10 minutes and could not be away from a toilet for any length of time. My parents and school teachers were advised to encourage me to train my bladder to hold more urine by withholding access to a toilet, which resulted in such severe pain and embarrassment that I became terrified of going to school and missed a significant amount of my primary school education.
“Coincidentally, recurrent ear infections throughout my childhood meant that I was prescribed numerous short courses of antibiotics, which somewhat helped to reduce my bladder symptoms. However, my symptoms would recur quickly after the antibiotic course was finished. Despite this clear correlation in symptoms, any suggestion of an infection was dismissed repeatedly by my GP.
“I battled through my teenage years with fluctuating bladder symptoms that often left me leaving the classroom several times during school lessons and avoiding school trips and social interaction for fear of suffering bladder symptoms. When I was 17, I suddenly developed a severe worsening of symptoms, resulting in immense burning during urination, severe urgency, severe bladder pain and a sensation that I had a boiling hot marble stuck in my urethra. I saw my GP, who diagnosed me with a UTI based on my symptoms and prescribed me with a week-long course of antibiotics. However, despite a slight improvement in my symptoms during this time, the symptoms continued to linger. When my GP subsequently sent my urine off for culture, it revealed mixed growth of doubtful significance, and I was diagnosed with “post-UTI irritation” and placed on oxybutynin. This pattern of events continued to repeat over the next 3 months, with numerous short 3-day courses of antibiotics, oxybutynin, Vesicare and amitriptyline being prescribed in an attempt to relieve my pain.
“Over the course of the next 2 years, my symptoms continued to worsen. I saw my GP hundreds of times and was referred to a total of two urogynaecologists and two urologists, all of whom either diagnosed me with overactive bladder or interstitial cystitis, and one of who claimed that my symptoms were psychological in nature and that my brain was simply “wired differently” to everyone else. I underwent two urodynamic studies, three KUB ultrasounds and two rigid cystoscopies under anaesthetic, the second of which I also underwent a ureteroscopy, retrograde study, urethral dilation, ureter dilation and bladder distension following a misdiagnosis of kidney stones after a poor-quality CT scan. Unfortunately, these investigations caused a massive deterioration in my symptoms and I was hospitalised on multiple occasions with severe uncontrollable pain and vomiting, kidney infections, urinary retention and passing frank blood clots that were so thick that I was unable to pass urine. Each time I was admitted to hospital and given IV antibiotics, my symptoms would improve dramatically, only to relapse as soon as the course had finished.
“By the time I self-referred to ***** private clinic in 2015, I was near suicidal with pain. My symptoms included severe, debilitating pain in my urethra, bladder, kidneys and vagina, urine retention that frequently left me unable to pass urine for 24 hours at a time, significant voiding issues and incredible urgency which felt as though my bladder was tying itself in knots. I frequently passed thick blood clots, and the immense urethral burning that plagued me with this condition felt as though someone had filled my urethra with petrol and set it on fire. I often awoke at night screaming with pain because the pain of leaking urine in my sleep was so terrifying that I often thought I was being attacked.
“[The clinic] diagnosed me with a chronic UTI via microscopy on a fresh, unspun urine sample and immediately placed me on an extended course of antibiotics. Although my progress has been slow as a result of so many years of inadequate treatment resulting in a deeply embedded infection, I have finally reached the stage where my symptoms are under control and I do not require the care of urologists or my GP with regards to my bladder symptoms. I am now able to live a relatively normal life with minimal bladder symptoms, and I have returned to work and university. However, as a result of the extensive strain that my untreated chronic UTI has placed on my autonomic nervous system over the past 16 years, I have been diagnosed with postural orthostatic tachycardia syndrome, inappropriate sinus tachycardia and gastrointestinal motility problems, thought to be due to gastroparesis, which are likely to be ongoing issues throughout my life.
“My greatest regret is that so many opportunities were missed to treat my symptoms when I was a child. Had I been given early access to treatment, my lifelong suffering could have been entirely preventable. I can only hope that in the future, children like myself will not be confined to the suffering and trauma that I have experienced.” [i]
[i] Malone-Lee, J., Cystitis Unmasked, 2021, pp241-244, tfm Publishing Limited, Castle Hill Barns, Harley, Shrewsbury, UK https://www.tfmpublishing.com/cystitis-unmasked